PCOS NICE guidelines overview
So I’m finally getting round to talking about the nice guidelines for PCOS. For those of you that may not know PCOS is an acronym for polycystic ovarian syndrome. To read more about this visit my previous blog post about PCOS here.
Disclaimer
I just want to start by saying that I am not a medical professional in any way shape or form and have just broken down the guidelines and explained some of the medical terms. You should always take the advice of your GP or seek a second opinion from a qualified clinician. Do not order medication from the internet just because you have found the name from this information. Any medication mentioned needs prescribing and monitoring carefully. Also I apologise in advance if this post seems really patronising. I don’t want to assume that people will necessarily know what all medical terms and abbreviations may be. So if you know this already I’m sorry if you don’t I hope I’ve helped. If you want to read it all go grab a cuppa and sit down. The first part summarises it very quickly. Here is a link to the guidelines themselves.
https://cks.nice.org.uk/polycystic-ovary-syndrome
Anyway. I wanted to start with some key take away pieces from the nice guidelines which are quick and easy to read. I’m going to focus on adults to begin with and highlight differences with adolescents afterwards. It’s worth mentioning before I start that these are only guidelines. It may be that your local health authority have a different policy for the treatment of PCOS. Your GP may or may not be aware of these guidelines so it can help to be armed with your own information.
Key information to take away
– Check for insulin resistance, diabetes type 2 and CVD (cardio vascular disease). Also worth having hormones checked and possible a uterine ultrasound.
– Treatment tends to be healthy lifestyle, weight loss and contraception.
– Metformin is not advised as treatment for PCOS unless type 2 diabetes is present. GPs are to refer patients to the hospital. Adolescents have a similar treatment pathway.
– There is a separate NICE guideline for fertility but it is advised to have a healthy lifestyle and lose weight in this guideline.
In depth information
Now a little more in depth.
> If you aren’t aware already you are at an increased risk for cardiovascular disease (CVD for short and will be referred to as this going forward) and type 2 diabetes. Due to this you will be encouraged to follow a healthy lifestyle.
> I’m sorry if you know this already but expect it from your GP. If you didn’t know that a well balanced diet and exercise could be beneficial. A healthy lifestyle can help with symptoms such as hyperinsulinism (high insulin levels) and hyperandrogegism (high male hormones). Lifestyle changes can also help to reduce the risk of CVD and type 2 diabetes. It has also been found to help with regulating the menstrual cycle and increases the chance of pregnancy if desired.
> You can ask for screening for the following tests:
– impaired glucose and type 2 diabetes screening
– CVD risk factors. These can include things such as blood pressure, Body mass index (BMI) and lipid levels, cholesterols etc.
> You must be asking for your hormone levels to be checked. LH, FSH, progesterone (be aware of where you are in your cycle). Also your testosterone, free androgen index and your sex hormone binding globulin (shbg).
> You will also be asked to stop smoking etc.
> You may want to think about snoring or daytime fatigue. It is possible that you have obstructive sleep apnoea and this can be treated separately if required.
> Something you may want to consider your emotional well being. A lot of women with PCOS can suffer with generalised anxiety and or depression. These can be due to a variety of reasons such as psychosexual, negative body image and also eating disorders. This is not an exhaustive list but possibly something you may want to consider when seeing your GP.
Management of PCOS
> In terms of the management of the clinical aspects
– Amenorrhea (lack of periods) you can be prescribed a progesterone tablet to induce a bleed. Usually this is a medroxyprogesterone at 10mg for 14 days. You could be referred for a ultrasound to check the uterus and the thickness of the endometrial lining. Especially if you haven’t had a period for a long time or have had unusual bleeding patterns.
– In order to reduce the risk of endometrial cancers etc it is advised that you should have a bleed every 3-4months. This can be by having an induced bleed or going on a contraceptive option.
– Again also a healthy lifestyle and lose weight. Yes there is a common theme 😂.
– Acne and hirsutism. The only recommendations from the nice guidelines and a healthy lifestyle along with weight loss.
Use of metformin and fertility support
> You Amy have heard about this wonder drug called metformin. Unfortunately it is worth highlighting that metformin and other insulin sensitising medications are NOT recommended by NICE. Research has found that there is little benefit from the use of these without evidence of diabetes. The levels of androgens are only decreased by 11% compared to a placebo. It also says that the GP should refer patients to the hospital and not prescribe metformin etc.
The same goes for fertility treatment. A healthy lifestyle and weight loss are the only things a GP can advise. They can refer onto the hospital, but many places require weight loss or specific BMI before treatment can begin. There is a separate set nice guidelines around fertility treatments.
Check out more information about this, it can be found at the following link.
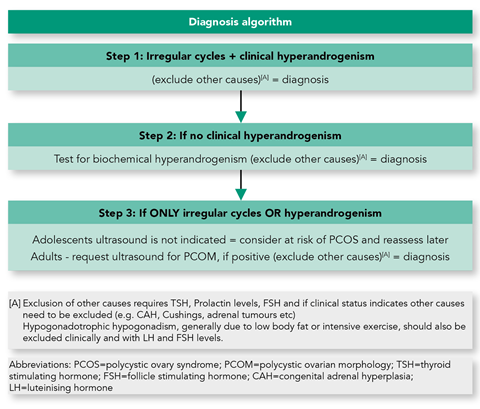
Diagnosing teenagers with PCOS type symptoms
In terms for differences with adolescents, there is only major one difference. This is that with girls who haven’t yet been diagnosed can be given contraception but they should be checked again. This is usually at full reproductive maturity which is deemed as 8 years post-menarche (after the first period). This usually involves coming off the contraception for 3 months and seeing what the symptoms are like after this time.
I hope these have helped someone. This has turned into a bit of a long one well done for making it this far. Next time I’m planning on looking at natural options. So if anyone has any thing they want to know about or have their own experiences please let me know. 😊
